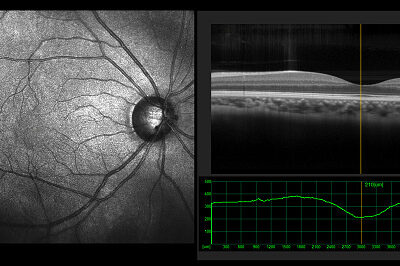
Optical Coherence Tomography – Heidelberg Spectralis
Optical coherence tomography (OCT) is a non-invasive imaging test. OCT uses light waves to take cross-sectional pictures of your retina as well as to image your optic disc and anterior segment.
RETINA OCT
With OCT, we can see each of the retina’s distinctive layers. This allows us to map and measure their thickness. These measurements help with diagnosis of disease. They also provide treatment guidance for multiple retinal conditions, including age-related macular degeneration, diabetic eye disease, aging/wrinkling of the macula, vitreous traction/detachment, retinal vascular occlusion and many others.
To prepare you for an OCT exam, we may or may not put dilating eye drops in your eyes. Dilating drops widen your pupil and make it easier to examine the retina.
You will sit in front of the OCT machine and rest your head on a support to keep it motionless. The equipment will then scan your eye without touching it. Scanning takes about 5 – 10 seconds per eye. If your eyes are dilated, they may be sensitive to light for several hours after the exam.
OPTIC DISC/GLAUCOMA OCT/also known as NERVE FIBER LAYER ANALYSIS
OCT is often used to help evaluate disorders of the optic nerve as well. The OCT exam helps your ophthalmologist see changes to the fibers of the optic nerve. For example, it can detect changes caused by glaucoma.
Our OCT contains the Comprehensive Glaucoma Module which allows for even more complete analysis of the layers of the retina and optic nerve and is the most detailed and accurate way to directly visualize the structures damaged by glaucoma. The software allows us to compare your eye to that of normal patients of similar age from a large database. This helps us determine if statistically your retina and optic nerve structures are normal and if not, where the problem lies. This adds tremendous precision to the OCT examination of glaucoma and other retinal and optic nerve diseases. It should aid in the rapid and accurate diagnosis and targeted treatment of these conditions. The test takes a little longer to perform but it is worth it for the level of increased information it can provide. Testing is completely non-contact and involves measuring light beams reflected off the back surface of your eye with advanced technology. It is completely safe and painless If you would like this test and you do not already have a diagnosis of Glaucoma, please inquire about scheduling the test for a modest fee as it would not be covered by insurance in that case.
ANTERIOR SEGMENT OCT
We also have the Anterior Segment module on our Spectralis machines. This allows detailed evaluation of the front part of the eye and is especially useful in evaluating Narrow Angle Glaucoma and the risk factors of this condition. The module helps us avoid placing a diagnostic contact lens on the eye, called Gonioscopy, therefore allowing for a NO TOUCH, NO CONTACT technique that is both more comfortable and safer.
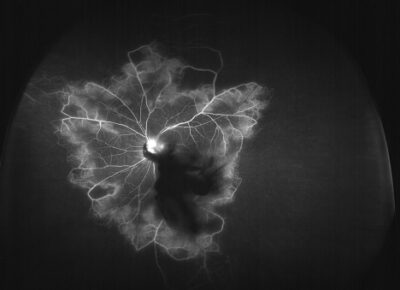 Flourescein Angiography
Flourescein Angiography
Fluorescein angiography (FA) is a diagnostic procedure done by our retina doctor in the office to study the dynamic circulation of the retina. During the procedure, pictures are taken to help her get a better look at the blood vessels and other structures in the back of the eye, to help her determine where to focus treatment. In our office, we use the Kowa VX-10 FA™.
FA is often recommended to find and diagnose and stage eye diseases, including:
• macular edema (swelling in the retina that distorts vision)
• diabetic retinopathy (damaged or abnormal blood vessels in the eye caused by diabetes)
• macular degeneration (age related changes to the visual center of the eye)
• blockage of veins and/or arteries inside the eye
• macular pucker (scar tissue on the surface of the retina)
FA is also used to:
• track changes in eye disease over time
• target treatment areas
FA is usually done in the office. It often takes less than 30 minutes. Here is what will happen:
The doctor or technician will put drops in your eyes to dilate (widen) your pupil. A yellowish colored dye (fluorescein) is injected in a vein, usually in your arm. It takes about 10–15 seconds for the dye to travel throughout your body. The dye eventually reaches the blood vessels in your eye, which causes them to “fluoresce,” or shine brightly. As the dye passes through your retina, a special camera takes pictures. The effects of dilating eye drops can last several hours and cause blurry vision and light sensitivity. Make sure to bring sunglasses to your appointment and have a driver take you home.
You may have some side effects from fluorescein angiography. You might notice that when you look at objects, they may seem dark or tinted. This side effect goes away in a few minutes. You may also notice that your skin may look a bit yellow. This happens because the dye travels to all of the veins in your body. Your skin will return to its normal color in a few hours. Other side effects include orange or dark yellow urine (for up to 48 hours afterwards) and a localized rash if dye leaks during the injection. Although it is rare, there are risks of an allergic reaction to the fluorescein dye. Patients who are allergic to the dye may experience hives or itchy skin. Very rarely, a person may have trouble breathing or other serious problems. Your doctor will be prepared to treat these kinds of allergic reactions with pills or intramuscular injections.
Fundus Photography -Zeiss Clarus Camera™
The fundus is the back of the eye and includes the retina, optic nerve, and retinal blood vessels.
Photography of this area can show drusen, abnormal bleeding, scar tissue, and areas of atrophy (or cell loss). Sometimes, with the Clarus camera, great pictures can be taken without the need to dilate the eye. This is a benefit for patients who are sensitive to dilating drops, or when the circumstances in a patient’s life make dilation challenging. The decision to dilate is a medical one to be made by the doctor at the time of service.
The entire procedure is brief, only taking a minute or two, and is painless. The patient puts his/her chin on the chin and forehead rests The technician will guide the patient where to look, and then take a picture. The light can be pretty bright, but it lasts a mere second. Some people have momentary dimming of vision from the bright light, but it returns to normal almost immediately. The information obtained from fundus photography is crucial to the doctor and his/her analysis and monitoring of your eye health.
Visual Field Testing – Haag Streit Octopus 600™
Peripheral vision is the part of your vision that allows you to sense your place in the world. Without peripheral vision, you would not be able see out of the corner of your eye, perceive motion properly, drive or navigate steps. People with certain medical conditions, such as glaucoma, or those taking high risk medications, such as Plaquenil, can be robbed of a portion of their peripheral or central vision, sometimes without them even knowing there is a loss or problem. Peripheral and central vision can be “mapped” by getting a visual field test. A visual field test is used by the doctor to determine if there is any defect in a patient’s peripheral vision, and then develop a plan of treatment based on the results.
We use the Haag Streit Octopus 600™ for our visual field testing. The patient is seated, with their forehead resting on a padded guide, and s/he is given a “clicker”. Looking straight ahead, the patient is presented with a series of light flashes, and presses the clicker for every flash s/he perceives. The test only takes a few minutes. There is no preparation for this test, and it is completely painless. The patient does need to be alert, capable of focusing on a fixed object within the machine, and capable of keeping their forehead on the fixed forehead guide unaided.
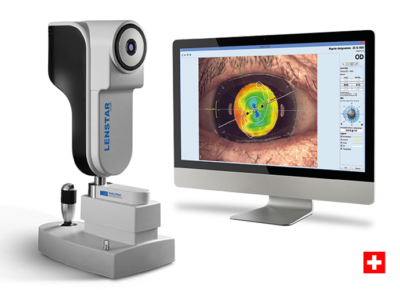
Intraocular Lens Implant Measurements – Haag-Streit LenStar 900™
When your cataract (the natural lens in your eye that becomes cloudy over time) needs to be surgically removed, the doctor will substitute in its place a tiny implant that essentially has your glasses prescription built into it. To pick the correct implant, the doctor will need to measure your eye for the appropriate implant. In our office, this is done primarily with the Lenstar 900, and sometimes with other measurement tests if your cataract is particularly dense. This is the latest technology in the advanced field of intraocular lens measurement devices, and we are proud to offer it to our patients.
The patient is seated in front of the device and puts their chin on the chin rest and forehead against the guide bar. The machine (and our technician) does the rest! It is painless and simply requires the patient to follow the technician’s instructions during the test. IT IS VITAL THAT IF YOU WEAR CONTACT LENSES YOU TELL OUR TECHNICIAN BEFORE THE TEST IS DONE. Based upon your measurements, the doctor will recommend a lens to you, after consulting with you as to how you wish to see after the cataract surgery. Please see Our Services section about small/no incision cataract surgery for a discussion about the various types of lens implants that Dr. Bannett uses.
We are fortunate to have the Haag Streit LENSTAR technology in our office. This remarkable machine directly measures with laser precision, the length and lens position of your eye to help predict the best implant for your eye. This combined with OPD (see section under MARCO Epic Refraction System) offers us the latest and most precise technology to help the most accurate results currently available. Realize of course that no combinations of machine and people exist that are 100%, but we get closer with each technological advancement, and updating and improving our technology and techniques is a constant commitment in our practice.
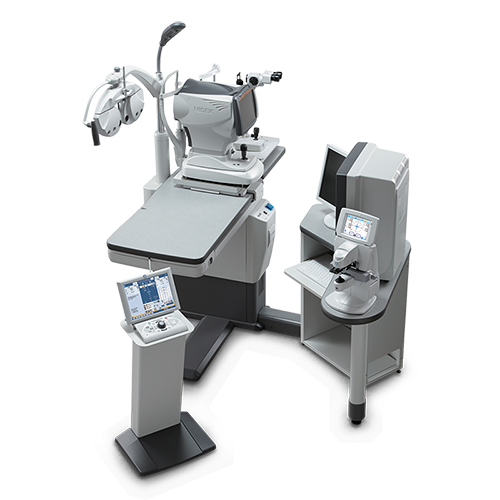
Marco EPIC™ Computerized Comprehensive Refraction System
If you are having vision complaints, such as can’t see to drive, difficulty reading/computer work or difficulty focusing/double vision, you will need a refraction. The refraction is that diagnostic test which asks the patient to make choices based on various lenses put in front of you, and usually results in a prescription for glasses. This test also gives the doctor the ability to determine whether new glasses will help you see better, and, importantly, when they won’t help you see better.
We use the Marco EPIC™ Refraction System. This comprehensive system offers greater patient satisfaction with refraction results and allows more time for technicians and physicians to focus on data assessment, diagnosis and prescribing final correction.
The Marco EPIC™ is revolutionary technology that replaces the standard refractor and allows us to control the entire refraction process from a keypad, moving the lenses quickly and accurately without any discomfort to you. With the Marco system, we can get a more accurate refraction, rather than using the “old-fashioned” way.
This EPIC™ system uses advanced computer and infrared technologies to help evaluate your unique visual needs. The patient will place their chin and forehead in the guides, and the technician will conduct the examination, which consists of obtaining objective and subjective data. During the subjective part of the examination, you will be presented with a variety of lens options, and will be asked which one you like better [“which is better, 1 or 2?”].
This system also contains a Corneal Wavefront Analyzer [OPD], which gives crucial information to the doctor about your own individual eye structure. This remarkable instrument involves directing light beams into the eye and measuring the effect your own optics have on the beam. The information obtained completely analyzes the refraction, distortion caused by the shape and position of your eye’s structures, and all aberrations in your ocular system. It measures and maps the shape and conformation of the cornea. Also it is an excellent way to analyze the quality of your tear film and the dryness of your eyes, all without direct physical contact. By measuring the geometry and optics of your eye with OPD, we are able to tell with greatly enhanced accuracy your suitability for Advanced Technology Implants available today to optimize your vision with cataract surgery. Dr. Bannett enjoys reviewing the OPD results with his patients in a discussion of the best way to approach your cataract treatment. In this way, your treatment is truly personalized to your exact needs.
B-scan Ultrasound – DGH Technology’s Scanmate™
B-scan ultrasound uses high frequency soundwaves that are transmitted from a probe/transducer into the eye. As these soundwaves strike the intraocular structures, an echo is reflected back to the probe and converted into an electrical signal. This signal is then reconstructed into a two-dimensional image on a monitor. The stronger the echo, the brighter the display. This process is repeated 1,000 times per second to produce a real-time display.
A B-scan allows the doctor to see retinal and vitreous detachments, masses in the eye, and various other pathologies. It is also used when a patient has a dense cataract, to allow the doctor to see the eye structures behind the cataract and get an idea if there is anything which might potentially limit the patient’s ability to have a good outcome after surgery.
A probe is glided over the surface of the closed eye by the doctor, who is simultaneously looking for pathology on the images on his/her computer screen.